Regulatory Bodies for Drug approval in India
The Drug and Cosmetic Act 1940 and Rules 1945 was enacted to regulate the import, manufacture, distribution and sale of drugs and cosmetics in India. The Central Drugs Standard Control Organization (CDSCO) is the regulatory body (as FDA in the USA) in India and drug controller general of India heads the CDSCO.
In 1988, the Indian parliament added Schedule Y to the Drug and Cosmetics Rules 1945. It provides the guidelines and requirements for clinical trials. It was further amended in 2005 to make it more aligned with international standard.
Definition of New drug :
Rule 122E under The Drug and Cosmetic Act 1940 and Rules 1945 defines the ‘new drug:
“drug, including bulk drugs substance (or phytopharmaceutical drug) which has not been used in the country to any significant extent under the conditions prescribed, recommended or suggested in its labelling and has not been recognised as effective and safe by the licensing authority for the proposed claims, drugs already approved for certain claims, which are now proposed to be marketed with modified or new claims (viz., new indications, dosage, dosage forms or routes of administration), or fixed-dose combinations of two or more drugs, individually approved earlier for certain claims, which are now proposed to be combined for the first time in a fixed ratio, or a new fixed ratio, with certain claims, (viz., indications, dosage, dosage forms or routes of administration)”
It is important to point out that “new drug shall continue to be considered as a new drug for a period of four years from the date of its first approval or its inclusion in the Indian Pharmacopoeia whichever is earlier”
Information and data required for approval of clinical trial and/or to import or manufacture of a new drug for marketing in India are clearly described in 122A, 122B and 122D, 122DA, 122DAA, 122E rules of Drugs and Cosmetics Rules and Appendix I, IA and VI of Schedule Y.
Form 29: Applicant/Sponsor has to take NOC from CDSCO. Based on this, the applicant can take license in form 29 from the state Licensing authority to manufacture test batches of new drugs (for development and generation of data).
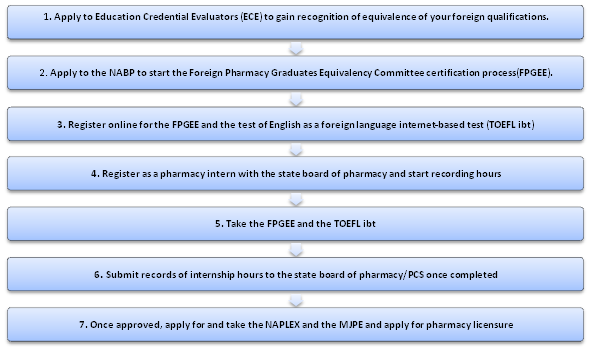
New Drug Approval Process in India:
- New drug candidate being developed in India and not Marketed anywhere else.
- New Drug candidate being developed outside India and not marketed anywhere in the world.
- If the drug is already approved/marketed in other countries but not approved in India.
- Drug candidate which are approved in other countries and being used from several years:
New drug Discovered in India and not Marketed anywhere else:
If a new substance is discovered in India and not approved in any part of the world, then all Phases of the trial (Phase I to Phase III) needs to be conducted to get the Market authorization.
New Drug candidate being developed outside India and not marketed anywhere in the world.
An applicant has to submit Phase I data along with the application. Licensing Authority reviews the Phase I data and Based on this, they may grant permission to conduct Phase II and subsequent Phase III trial in India concurrently with another global trial of a drug candidate. It is also possible that regulatory authority may ask to repeat the Phase I trial in India.
If the drug is already approved/marketed in other countries but not approved in India.
- In general, if a drug candidate is approved in one or more countries like USA, UK, Canada, European Union, Japan, and Australia, then it will be considered for approval of manufacture/import and marketing in India.
- If the sponsor is seeking approval of the drug candidate in India which is already have been approved/Marketed in other countries, then sponsor or applicant has to conduct Phase 3 data on at least 100 subjects across 3 to 4 centre to confirm the safety and efficacy of drug candidate in Indian population.
- The regulatory authority may ask any additional non-clinical and clinical data based on the nature of drug candidate and information available
It is important to note that if a drug candidate is discovered in India and it is not marketed in any other countries, then the applicant has to conduct Phase 3 studies in 500 subjects across 10 to 15 centre.
Scenarios when clinical trials are not required to be conducted for drug approval in India
If the drug is approved in other countries and applicant is seeking approval to market/manufacture/import this drug in India then it is not necessary to conduct clinical trials in India if drug candidate meets any of the following requirements.
The requirement of submitting results of local clinical trials may not be necessary As per the provisions given in the Drugs & Cosmetics Rules.
- serious/life-threatening condition,
- Diseases which carries special relevance in Indian Population
- No satisfactory therapeutic option available
- Unmet medical need exist
- Rare Disease
- If a drug candidate offers added a significant advantage over the existing treatment options for a specific disease
Drug candidate which are approved in other countries and being used from several years:
In this case, a clinical trial may be waived off in India as per rule 122 A of drug and cosmetic Act if the sufficient published safety data is available, however, how many years will be considered as “ several years” is not clear.
Important facts:
Category A: Clinical trial (approved in the U.S., Britain, Switzerland, Australia, Canada, Germany, South Africa, Japan and the European Union) are eligible for fast-tracking. Because these clinical trials have been approved already by a competent and robust process by a well developed regulatory framework, so the India regulatory authorities can rely on data to some extent for dug approval in India.
Category B: Apart from above, All trial falls under B. India Regulatory authority reviews the data and scrutiny process takes 16-18 weeks.
Investigational New Drug Application (IND): Data of chemistry, manufacturing, control and animal studies needs to be submitted to regulatory authority along with other documents such as protocol, investigator’s brochures (IB), and informed consent documents. A copy of this application needs to be submitted to the ethical committee as well. DCGI reviews this application and applicant can conduct a clinical trial in India once it gets approval for this.
New Drug Application: New Drug Registration using form 44 along-with preclinical, clinical and other relevant data such as marketing status in other countries, testing protocol, label, product monograph, needs to be submitted to the regulatory agency. It may take 12-18 months to review the application.
Approval of Drugs in India, with some modification over existing approved drug
Pharmaceutical companies may change an already approved product in many ways namely:
- New proposed Indications
- Change in dosage
- dosage form (including sustained release dosage form)/formulation change
- Route of administration (ie oral from IV)
This type of application differs from the New drug applications as in this case, drug regulatory agency relies on safety and efficacy data of already approved drug at least in part.
Please note this pathway or application is like an sNDA in The regulatory authority may ask some additional clinical or non-clinical data which is decided by case by case basis.
In the below scenario, the regulatory authority may require less or no additional data of Animal Pharmacological, Animal Toxicological and clinical studies.
- If the drug is already approved by other countries for the proposed indication
- Availability of evidence showing no difference in the metabolism of the drug due to ethnic differences
- Clinical data is available supporting benefit-risk ratio in favour of drug candidate for the proposed new claim
- Package insert from other countries shows that there is no new safety concern if the drug is given to the Indian patient for the new claim.
- if new claim covers serious or life-threatening diseases or any disease which are quite relevant to India
Note: Comparative clinical trials and bio-equivalence study comparing the modified release formulation with the immediate-release formulation is required to be conducted if the applicant seeks approval for Modified release product. In case if the proposed formulation is already approved then comparative bio-equivalence study is recommended. Further guidance can be sought from CDSCO.
You can follow the blog of Fixed-Dose Combination Approval Process to have a better understanding of how India is approving fixed-dose combination.
Ref: https://journals.sagepub.com/doi/full/10.1177/0971721818762931
http://www.globalresearchonline.net/journalcontents/v13-2/004.pdf
https://cdsco.gov.in/opencms/opencms/en/Home/