December 07, 2021: “Liver-targeted antisense therapy in Phase III development for the treatment of transthyretin amyloidosis, a systemic, progressive and fatal condition
AstraZeneca has entered into a new global development and commercialisation agreement with Ionis Pharmaceuticals, Inc. (Ionis) for eplontersen, formerly known as IONIS-TTR-LRX.
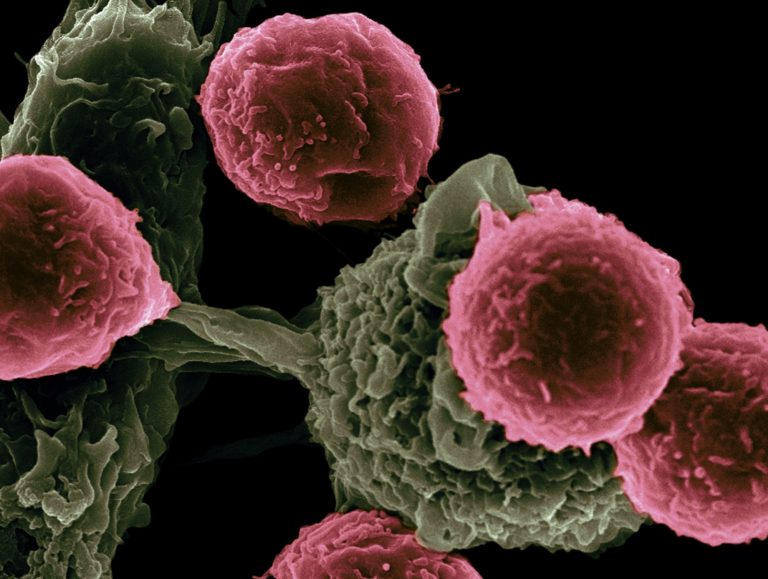
Eplontersen is a ligand-conjugated antisense investigational medicine currently in Phase III clinical trials for amyloid transthyretin cardiomyopathy (ATTR-CM) and amyloid transthyretin polyneuropathy (ATTR-PN).
It is designed to reduce the production of transthyretin (TTR protein) to treat both hereditary and non-hereditary forms of TTR amyloidosis (ATTR).
The companies will jointly develop and commercialise eplontersen in the US, while AstraZeneca will develop and commercialise it in the rest of the world, except in Latin America.
ATTR-CM is a systemic, progressive and fatal condition that leads to progressive heart failure and death within four years from diagnosis.
It remains underdiagnosed and its prevalence is thought to be underestimated due to a lack of disease awareness and the heterogeneity of symptoms.
Hereditary ATTR-PN is a debilitating disease that leads to peripheral nerve damage with motor disability within five years of diagnosis and, without treatment, is generally fatal within a decade.
Mene Pangalos, Executive Vice President, BioPharmaceuticals R&D, AstraZeneca, said: “Eplontersen has the potential to halt the progression of TTR-mediated amyloidosis, irrespective of whether it’s caused by genetic mutations or aging.
Thanks to its precise liver-targeting properties, it also has the potential to be a best-in-class treatment for patients suffering from this devastating disease and who currently have limited options.”
Hereditary ATTR-PN is expected to be the first indication for which the companies will seek regulatory approval for eplontersen, with the potential to file a new drug application with the US Food and Drug Administration by the end of 2022.
Financial considerations
AstraZeneca will pay Ionis an upfront payment of $200m and additional conditional payments of up to $485m following regulatory approvals.
It will also pay up to $2.9bn of sales-related milestones based on sales thresholds between $500m and $6bn, plus royalties in the range of low double-digit to mid-twenties percentage depending on the region.
The collaboration includes territory-specific development, commercial and medical affairs cost-sharing provisions.
The transaction will be funded with cash and is expected to be neutral to Core earnings in 2021.
It will be accounted for as an intangible asset acquisition, recognised initially at the upfront amount, with any potential future milestone payments capitalised into the intangible asset as they are recognised.
Ionis will continue to manufacture and supply eplontersen for the existing clinical studies and process qualification.
AstraZeneca will be responsible for commercial supply, with transition timing to be agreed by both parties. AstraZeneca will book all sales generated under the agreement.
The transaction is expected to close in the fourth quarter of 2021, subject to customary closing conditions and regulatory clearances. The transaction does not impact the AstraZeneca’s financial guidance for 2021.”