December 07, 2021: “Roche announced that the European Commission has extended the marketing authorisation for Actemra®/RoActemra® (tocilizumab) to include the treatment of COVID-19 in adults who are receiving systemic corticosteroids and require supplemental oxygen or mechanical ventilation.
This decision comes just hours after the recommendation by the European Medicines Agency’s (EMA) Committee for Medicinal Products for Human Use (CHMP), reflecting the urgent need for Actemra/RoActemra as a potential treatment option during the COVID-19 public health emergency.
“Actemra/RoActemra is the second Roche medicine to have received rapid European Commission approval in COVID-19 in recent weeks,” said Levi Garraway, M.D., Ph.D., Roche’s Chief Medical Officer and Head of Global Product Development.
“The totality of evidence shows that Actemra/RoActemra can benefit those suffering with severe COVID-19.
Together with vaccines, other treatments and testing, Actemra/RoActemra forms an important piece of the care puzzle as we confront new challenges of the pandemic in Europe and around the world.”
The decision from the European Commission follows an accelerated assessment by the EMA’s CHMP, which reviewed results from four studies of Actemra/RoActemra in over 5,500 patients with severe or critical COVID-19.
These include the Roche-led phase III COVACTA, EMPACTA and REMDACTA trials, and the University of Oxford’s Randomised Evaluation of COVID-19 Therapy (RECOVERY) study, which was supported by Roche.
Outside of the European Union, Actemra/RoActemra has been provisionally approved in Australia, authorised for emergency use in the United States and Ghana, and recommended by the World Health Organization (WHO) for the treatment of COVID-19.
Roche is working closely with regulatory bodies and other partners around the world on the next steps to bring this medicine to as many people as possible.
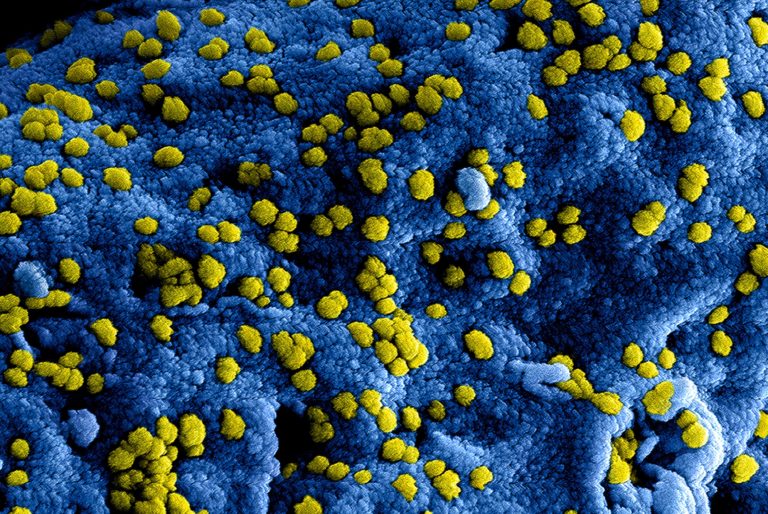
Following the recent emergence of the new SARS-CoV-2 variant of concern, Omicron (B.1.1.529), WHO has reported that interleukin 6 receptor blockers, such as Actemra/RoActemra, are expected to still be effective for managing patients with severe COVID-19.
In these exceptional times, we stand together with society, governments, healthcare providers and all those working towards the common goal of overcoming the COVID-19 pandemic.
About Actemra®/RoActemra® (tocilizumab) in COVID-19 clinical trials
Roche has evaluated Actemra/RoActemra in COVID-19 in three phase III randomised studies: COVACTA, EMPACTA and REMDACTA.
COVACTA was a global, randomised, double-blind, placebo-controlled phase III study (COVACTA, NCT04320615), which evaluated the safety and efficacy of intravenous Actemra/RoActemra plus standard of care in adult patients hospitalised with severe COVID-19 pneumonia compared to placebo plus standard of care.
The primary and secondary endpoints included clinical status, mortality, mechanical ventilation and intensive care unit (ICU) variables. Patients were followed for 60 days post-randomisation.
EMPACTA (Evaluating Minority Patients with Actemra) was a phase III, randomised, double-blind, placebo-controlled multicentre study (EMPACTA, NCT04372186) which evaluated the efficacy and safety of Actemra/RoActemra in the treatment of COVID-19 pneumonia among hospitalised patients that are often underrepresented in clinical trials.
The primary endpoint was the cumulative proportion of participants dying or requiring mechanical ventilation by Day 28. Secondary endpoints included: time to clinical failure (defined as the time to death), mechanical ventilation, ICU admission, or withdrawal (whichever occured first); mortality rate by Day 28; and time to hospital discharge or “ready for discharge.”
REMDACTA was a two-armed global phase III, randomised, double-blind, multicentre study (REMDACTA, NCT04409262) to evaluate the efficacy and safety of Actemra/RoActemra plus Veklury® (remdesivir), versus placebo plus Veklury in hospitalised patients with severe COVID-19 pneumonia receiving standard of care.
Veklury is an antiviral medicine that works to stop replication of SARS-CoV-2, the virus that causes COVID-19.
The REMDACTA trial was conducted in collaboration with Gilead Sciences, Inc.
The primary endpoint was improvement in time to hospital discharge by Day 28.
Key secondary endpoints included likelihood of death, likelihood of progression to mechanical ventilation or death, and clinical status. Clinical status was measured by the 7-category ordinal scale, which tracks patients’ clinical status based on the need for intensive care and/or ventilator use, as well as supplemental oxygen requirements.
Patients were followed for 60 days post-randomisation.
There have also been a number of clinical trials with an external third party as the sponsor exploring the efficacy and safety of Actemra/RoActemra for the treatment of patients hospitalised with COVID-19, including the University of Oxford’s RECOVERY study, which was supported by Roche.
RECOVERY was a phase III, randomised trial (NCT04381936), which evaluated whether multiple potential treatments, including Actemra/RoActemra, prevent death in hospitalised adult patients with severe COVID-19.
Results of a prospective meta-analysis of almost 11,000 patients across 27 clinical trials, published by researchers from the World Health Organization in The Journal of the American Medical Association, found that treatment of hospitalised patients with severe or critical COVID-19 with IL-6 receptor blockers, including Actemra/RoActemra, was associated with improved mortality and reduced progression to invasive mechanical ventilation or death compared with usual care or placebo.
The prospective meta-analysis included data on Actemra/RoActemra in COVID-19 from COVACTA, EMPACTA and REMDACTA, along with 16 additional third-party studies.
About Actemra®/RoActemra® (tocilizumab)
Actemra/RoActemra was the first approved anti-IL-6 receptor biologic and is available in both intravenous (IV) and subcutaneous (SC) formulations for the treatment of adult patients with moderate-to-severe active rheumatoid arthritis (RA).
Actemra/RoActemra can be used alone or with methotrexate (MTX) in adult RA patients who are intolerant to, or have failed to respond to, other disease-modifying anti-rheumatic drugs (DMARDs).
In Europe, RoActemra IV and SC are also approved for use in adult patients with severe, active and progressive RA who previously have not been treated with MTX.
Actemra/RoActemra IV and SC are also approved globally for polyarticular juvenile idiopathic arthritis (pJIA) and systemic juvenile idiopathic arthritis (sJIA) in children two years of age and older.
Actemra/RoActemra SC is approved globally for giant cell arteritis (GCA), and Actemra/RoActemra IV is approved for the treatment of chimeric antigen receptor (CAR) T-cell-induced severe or life-threatening cytokine release syndrome (CRS) in people two years of age and older.
Actemra/RoActemra was the first approved treatment for sJIA, GCA and CRS. Actemra SC is now approved in the United States for slowing the rate of decline in pulmonary function in adult patients with systemic sclerosis-associated interstitial lung disease (SSc-ILD).
In addition to the above-mentioned indications, in Japan Actemra IV is also approved for the treatment of Castleman’s disease and adult Still’s disease, and the Actemra SC formulation is approved for Takayasu arteritis.
RoActemra is also approved in Europe for the treatment of COVID-19 in adults who are receiving systemic corticosteroids and require supplemental oxygen or mechanical ventilation.
Actemra/RoActemra is part of a co-development agreement with Chugai Pharmaceutical Co., Ltd and has been approved in Japan since April 2005. Actemra/RoActemra is approved in more than 110 countries worldwide.”
https://www.roche.com/media/releases/med-cor-2021-12-07.htm