December 20, 2021: “EMA has recommended granting a conditional marketing authorisation for Novavax’s COVID-19 vaccine Nuvaxovid (also known as NVX-CoV2373) to prevent COVID-19 in people from 18 years of age.
Nuvaxovid is the fifth vaccine recommended in the EU for preventing COVID-19. It is a protein-based vaccine and, together with the already authorised vaccines, will support vaccination campaigns in EU Member States during a crucial phase of the pandemic.
After a thorough evaluation, EMA’s human medicines committee (CHMP) concluded by consensus that the data on the vaccine were robust and met the EU criteria for efficacy, safety and quality.
Results from two main clinical trials found that Nuvaxovid was effective at preventing COVID-19 in people from 18 years of age.
The studies involved over 45,000 people in total. In the first study, around two thirds of participants received the vaccine and the others were given a placebo (dummy) injection; in the other study, participants were equally split between Nuvaxovid and placebo.
People did not know if they had been given Nuvaxovid or placebo.
The first study, conducted in Mexico and the United States, found a 90.4% reduction in the number of symptomatic COVID-19 cases from 7 days after the second dose in people who received Nuvaxovid (14 cases out of 17,312 people) compared with people given placebo (63 out of 8,140 people). This means that the vaccine had a 90.4% efficacy in this study.
The second study conducted in the United Kingdom also showed a similar reduction in the number of symptomatic COVID-19 cases in people who received Nuvaxovid (10 cases out of 7,020 people) compared with people given placebo (96 out of 7,019 people); in this study, the vaccine efficacy was 89.7%.
Taken together, the results of the two studies show a vaccine efficacy for Nuvaxovid of around 90%. The original strain of SARS-CoV-2 and some variants of concern such as Alpha and Beta were the most common viral strains circulating when the studies were ongoing.
There is currently limited data on the efficacy of Nuvaxovid against other variants of concern, including Omicron.
The side effects observed with Nuvaxovid in the studies were usually mild or moderate and cleared within a couple of days after vaccination. The most common ones were tenderness or pain at the injection site, tiredness, muscle pain, headache, a general feeling of being unwell, joint pain, and nausea or vomiting.
The safety and effectiveness of the vaccine will continue to be monitored as it is used across the EU, through the EU pharmacovigilance system and additional studies by the company and European authorities.
Table of Contents
Where to find more information
The product information for Nuvaxovid contains information for healthcare professionals, a package leaflet for members of the public and details of conditions of the vaccine’s authorisation.
An assessment report with details of EMA’s evaluation of Nuvaxovid and the full risk management plan will be published shortly.
Clinical trial data submitted by the company in the application for marketing authorisation will be published on the Agency’s clinical data website in due course.
More information is available in an overview of the vaccine in lay language, including a description of the vaccine’s benefits and risks and why EMA recommended its authorisation in the EU.
How Nuvaxovid works
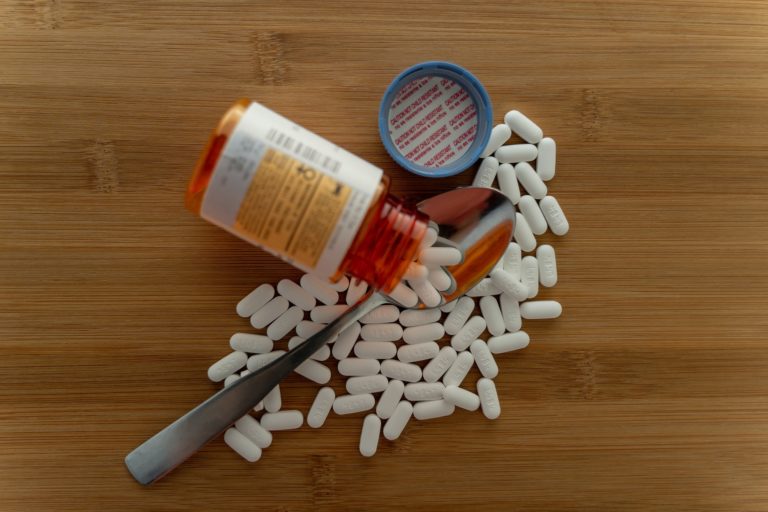
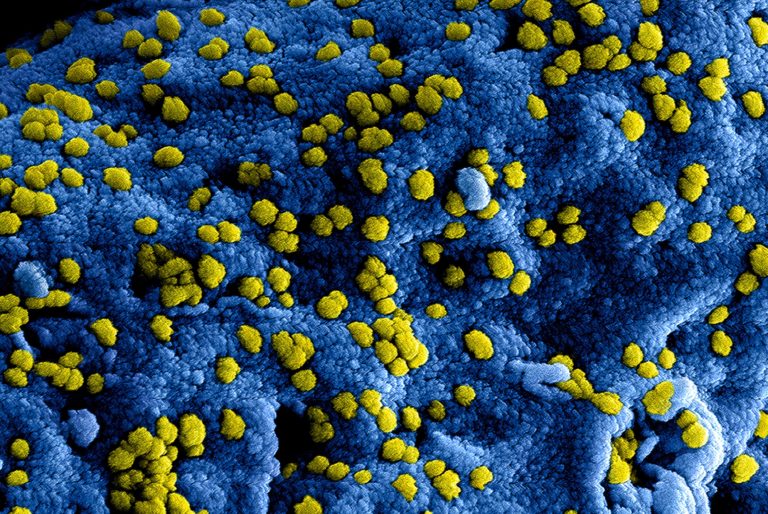
Nuvaxovid works by preparing the body to defend itself against COVID-19. The vaccine contains a version of a protein found on the surface of SARS-CoV-2 (the spike protein), which has been produced in the laboratory. It also contains an ‘adjuvant’, a substance to help strengthen the immune responses to the vaccine.
When a person is given the vaccine, their immune system will identify the protein as foreign and produce natural defences — antibodies and T cells — against it.
If, later on, the vaccinated person comes into contact with SARS-CoV-2, the immune system will recognise the spike protein on the virus and be prepared to attack it.
The antibodies and immune cells can protect against COVID-19 by working together to kill the virus, prevent its entry into the body’s cells and destroy infected cells.
Nuvaxovid is given as two injections, usually into the muscle of the upper arm, 3 weeks apart.
Conditional marketing authorisation
The European Commission will now fast-track the decision-making process to grant a decision on the conditional marketing authorisation for Nuvaxovid, allowing this vaccine to be included in vaccination programmes rolled out across the EU.
Conditional marketing authorisation (CMA) is used as the fast-track authorisation procedure to speed up approval of treatments and vaccines during public health emergencies in the EU. CMAs allow authorisation of medicines that fulfil an unmet medical need on the basis of less complete data than normally required.
This happens if the benefit of a medicine or vaccine’s immediate availability to patients outweighs the risk inherent in the fact that not all the data are yet available.
A CMA guarantees that the approved medicine or vaccine meets rigorous EU standards for efficacy, safety and quality and is manufactured in approved, certified facilities in line with high pharmaceutical standards for large-scale production.
Once a CMA has been granted, companies must provide further data from ongoing or new studies within pre-defined deadlines to confirm that the benefits continue to outweigh the risks.
Monitoring the safety of Nuvaxovid
In line with the EU’s safety monitoring plan for COVID-19 vaccines, Nuvaxovid will be closely monitored and subject to several activities that apply specifically to COVID-19 vaccines.
Although large numbers of people have received COVID-19 vaccines in clinical trials, certain side effects may only emerge when millions of people are vaccinated.
Companies are required to provide monthly safety reports in addition to the regular updates required by legislation and conduct studies to monitor the safety and effectiveness of the vaccines as they are used by the public.
In addition, independent studies of COVID-19 vaccines coordinated by EU authorities will give more information on the vaccine’s long-term safety and benefit in the general population.
These measures will allow regulators to swiftly assess data emerging from a range of different sources and take any necessary regulatory action to protect public health.
Assessment of Nuvaxovid
During the assessment of Nuvaxovid, CHMP had the support of EMA’s safety committee, PRAC, who assessed the risk management plan of Nuvaxovid, and the COVID-19 EMA pandemic task force (COVID-ETF), a group that brings together experts from across the European medicines regulatory network to facilitate rapid and coordinated regulatory action on medicines and vaccines for COVID-19.”
https://www.ema.europa.eu/en/news/ema-recommends-nuvaxovid-authorisation-eu