April 19, 2022: “GlaxoSmithKline plc announced that the USFDA accepted the NDA for daprodustat, an oral hypoxia-inducible factor prolyl hydroxylase inhibitor (HIF-PHI), for the potential treatment of patients with anaemia of chronic kidney disease (CKD).
Daprodustat was developed based upon the unique Nobel Prize-winning science that demonstrated how cells sense and adapt to oxygen availability.
The FDA has assigned a Prescription Drug User Fee Act (PDUFA) action date of 1 February 2023.
The daprodustat NDA is based on positive results from the ASCEND phase III clinical trial programme, which included five pivotal trials assessing the efficacy and safety of daprodustat for the treatment of anaemia across the spectrum of CKD.
Results from the key cardiovascular outcomes trials were published in the New England Journal of Medicine in November 2021 and included non-dialysis (ASCEND-ND) and dialysis (ASCEND-D) CKD patients.
These trials demonstrated that daprodustat improved and/or maintained haemoglobin (Hb) within the target level (10-11.5 g/dL) without increased major adverse cardiovascular events (MACE) in the intention-to-treat (ITT) populations in each pivotal study, when compared to the standard of care, an erythropoietin stimulating agent (ESA), across both non-dialysis and dialysis patient settings.
Daprodustat is currently approved in Japan as Duvroq for patients with renal anaemia.
In March 2022, the European Medicines Agency (EMA) validated the marketing authorisation application (MAA) for daprodustat, which is currently under review. Additional regulatory filings are anticipated to continue throughout 2022.
About the ASCEND phase III clinical trial programme
The ASCEND programme includes five phase III trials to assess the efficacy and safety profile of daprodustat for treating anaemia of CKD across the disease pathway.
The programme enrolled over 8,000 patients treated for up to 4.26 years. Results from all five trials were presented at the American Society of Nephrology’s Kidney Week 2021.
Results from the two pivotal cardiovascular outcomes trials, ASCEND-ND and ASCEND-D, which investigated patients not on dialysis and on dialysis, respectively, were also published in the New England Journal of Medicine:
- ASCEND-ND (Anaemia Studies in CKD: Erythropoiesis via a Novel PHI Daprodustat-Non-Dialysis) enrolled 3,872 non-dialysis dependent patients with anaemia of CKD who were either switched from the standard of care (ESA) or not currently receiving ESA therapy to receive daprodustat or ESA control (darbepoetin alfa).
Iron management protocols were instituted across both arms of the trial.
The trial met its primary efficacy and safety endpoints. Results showed that daprodustat improved and/or maintained Hb within the target level (10-11.5 g/dL) for these patients, and the primary safety analysis of the ITT population showed that daprodustat achieved non-inferiority of MACE compared to ESA control. - ASCEND-D (Anaemia Studies in CKD: Erythropoiesis via a Novel PHI Daprodustat-Dialysis) enrolled 2,964 dialysis patients with anaemia of CKD who were switched to receive daprodustat or ESA control from a standard of care ESA therapy.
A uniform iron management protocol was instituted across both arms of the trial. The trial met its primary efficacy and safety endpoints.
Results showed daprodustat improved or maintained Hb within target levels (10-11.5 g/dL) for these patients, and the primary safety analysis of the ITT population showed that daprodustat achieved non-inferiority of MACE compared to ESA control.
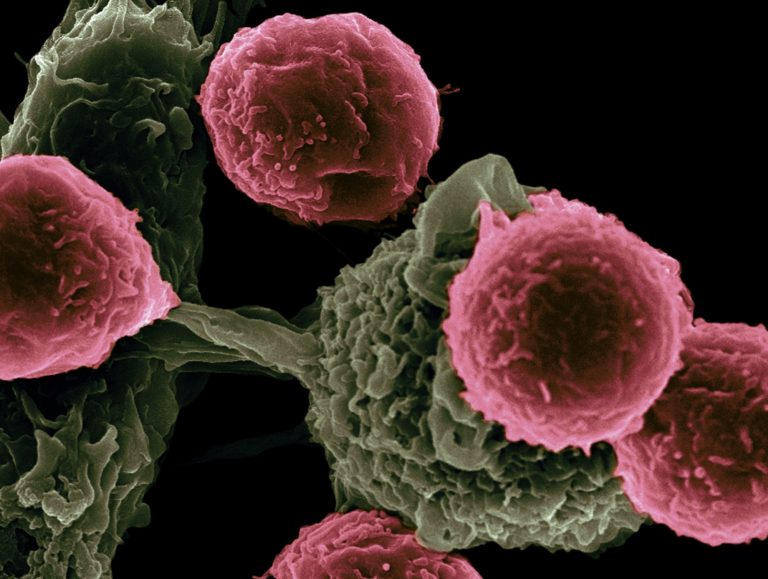
About anaemia of chronic kidney disease
CKD, characterised by progressive loss of kidney function, is an increasing global public health burden.
Risk factors for CKD include hypertension, diabetes, obesity and primary renal disorders.
Furthermore, CKD is an independent risk factor for cardiovascular disease.
Anaemia is an important and frequent complication of CKD. However, it is often poorly diagnosed and undertreated in patients with early-stage CKD, such as those not on dialysis.
Over 700 million patients suffer from CKD worldwide, and an estimated 1-in-7 of these patients have anaemia.
When left untreated or undertreated, anaemia of CKD is associated with poor clinical outcomes and leads to a substantial burden on patients and healthcare systems.
About daprodustat
Daprodustat, a HIF-PHI, belongs to a novel class of oral medicines indicated for the potential treatment of anaemia of CKD in adult patients not on dialysis and on dialysis.
Inhibition of oxygen-sensing prolyl hydroxylase enzymes stabilises hypoxia-inducible factors, which can lead to transcription of erythropoietin and other genes involved in the correction of anaemia, similar to the physiological effects that occur in the human body at high altitude.
Daprodustat has been developed to provide a convenient oral treatment option for patients with anaemia of CKD.”