June 23, 2022: “Detailed results from the positive FoCus Phase III trial in Wilson disease showed that ALXN1840, an investigational once-daily, oral medicine, met its primary endpoint demonstrating three-times greater copper mobilisation from tissues compared to the standard of care (SoC) arm (Least Square Mean Difference [LSM Diff] 2.18 µmol/L; p< 0.0001), including in patients who had been treated previously for an average of 10 years.1
In the trial, people taking ALXN1840 experienced rapid copper mobilisation, with a response at four weeks and sustained through 48 weeks.
Results from the trial will be presented on 23 June at the 2022 International Liver Congress (ILC) in London.
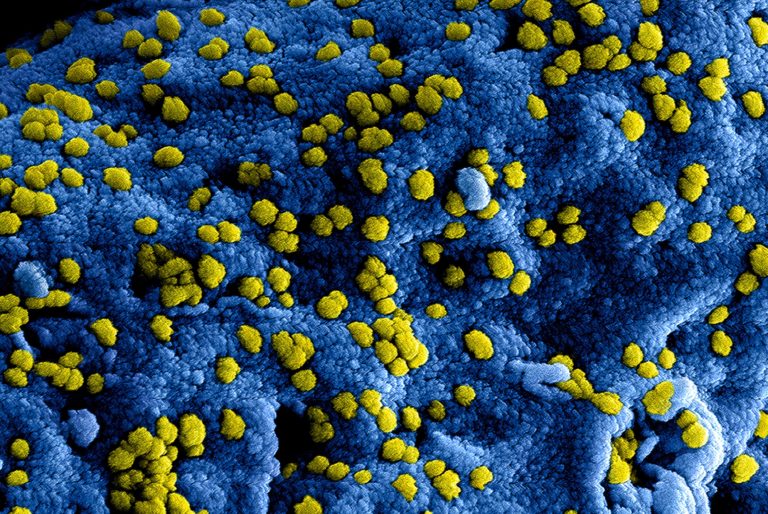
Wilson disease is a rare and progressive genetic condition in which the body’s pathway for removing excess copper is compromised.
This may result in the accumulation of copper in a person’s liver, brain or other vital organs. Damage from excess copper build-up in tissues and organs may lead to symptoms of liver, neurological and psychiatric diseases, which may be irreversible.
Even after SoC treatment is initiated, some patients experience worsening of disease, especially of neurologic symptoms.
Change in neurological scale scores and clinician-reported functional assessments with ALXN1840 treatment were also evaluated in a post-hoc analysis as secondary endpoints in the Phase III trial.
In patients who were symptomatic at baseline, there were greater improvements in neurological scores for those treated with ALXN1840 compared to SoC (Unified Wilson Disease Rating Scale [UWDRS] part II symptomatic ALXN1840 -1.7, SoC -0.8; UWDRS Part III symptomatic ALXN1840 -2.91, SoC -1.31). However, there were no significant differences between treatment groups observed at 48 weeks.1
Most patients in the trial had low symptom scores at baseline, so there was minimal room for total score improvement (UWDRS Part II ALXN1840 -0.6, SoC -0.3; UWDRS Part III ALXN1840 -2.20, SoC -1.02).
As people with Wilson disease experience a highly varied degree of symptoms4, this total score may not reflect the extent of disease severity.
ALXN1840 was well tolerated and the long-term safety and efficacy of ALXN1840 is being assessed in an up to 60-month extension period.1
Professor Karl Heinz Weiss, MD, Director of the Department of Internal Medicine at Salem Medical Centre Heidelberg and investigator in the FoCus Phase III trial, said: “These data from the largest global trial in Wilson disease to date show significant copper mobilisation from the tissues with ALXN1840, even in patients who were on standard of care for over a decade on average.
These results have the potential to reframe the way doctors can think about the disease given that current therapies focus on removing copper from the blood.
We are also encouraged by initial neurological improvement with ALXN1840 in those who were symptomatic and believe that assessing individual patient experiences may provide a better understanding of the impact on daily life.”
Marc Dunoyer, Chief Executive Officer, Alexion, said: “Many people with Wilson disease continue to experience symptoms even after years of intervention with current therapies, illuminating an urgent need to re-evaluate the standard of care.
Applying our 30 years of experience in rare disease clinical development, Alexion has conducted rigorous scientific research to bring fresh thinking to Wilson disease around the importance of copper mobilisation from the tissues.
These data further our efforts to potentially introduce a novel treatment for patients who have gone decades without meaningful innovation.”
Summary of efficacy and safety results
The primary endpoint gauged the daily mean Area Under the Effect Curve (AUEC) for directly measured non-ceruloplasmin-bound copper (dNCC)ii over 48 weeks.
The dNCC parameter includes copper bound in an inert complex with ALXN1840.”