Feb
28, 2020: The U.S. FDA has
approved an application for the first generic of Daraprim (pyrimethamine)
tablets for the treatment of toxoplasmosis (an infection caused by the parasite
Toxoplasma gondii) when used with a sulfonamide (a group of medicines used to
treat bacterial infections).
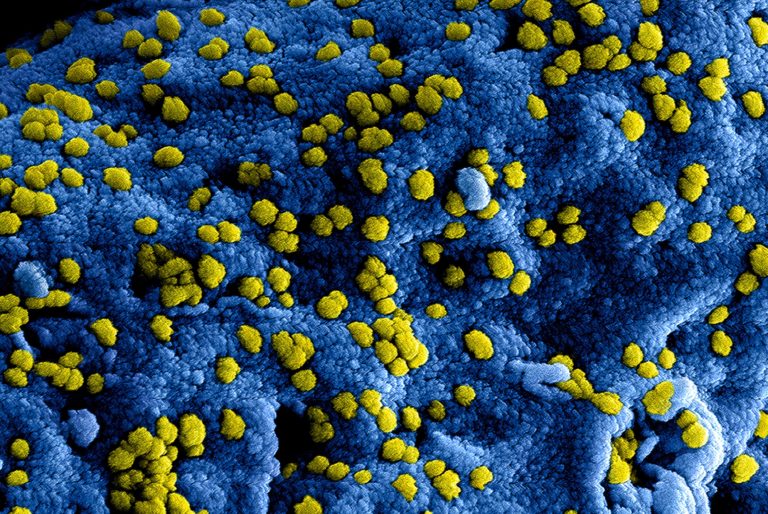
Toxoplasmosis is an infection
caused by a single-celled parasite named Toxoplasma gondii that can cause
brain, eye or other organ damage if severe. A toxoplasma infection can occur,
inter alia, by eating undercooked, contaminated meat or shellfish; drinking
water contaminated with toxoplasma; or by accidental swallowing of the parasite
through contact with toxoplasma-containing cat feces. It is considered the
leading cause of death in the United States due to foodborne disease.
In pregnant women and people with weak immune systems, such
as those with HIV or AIDS, those undergoing other forms of chemotherapy and
those who have recently received an organ transplant, serious toxoplasmosis is
more likely. However, even people with healthy immune systems can occasionally
experience toxoplasmosis damage to the eyes.One focus area under the action
plan is to improve the efficiency of the generic drug production, review and
approval process, and to close loopholes that allow brand-name drug companies
to avoid generic competition.
As part of these
important efforts, the FDA maintains a list of off-patent, off-exclusivity drug
products without an approved generic in order to improve transparency and support
the development and submission of applications for drugs with limited
competition. Pyrimethamine is incorporated on this list. The FDA also
prioritizes the review of the submissions for generic drugs for which there are
fewer than three approved generic versions for the reference listed drug (RLD)
and for which there are no blocking patents or exclusivities on the RLD.
In addition, certain “gaming” tactics have been used at times to delay
generic competition. One example is when brand-name drug manufacturers attempt
to prevent potential generic applicants from obtaining samples of the certain
medicines necessary to support approval of a generic drug application. To
increase clarity on this subject, the FDA posted a list describing all drugs
for which a prospective generic applicant has received an inquiry concerning
the limited distribution of the reference drug. Daraprim appears on this chart.
The most common side
effects for pyrimethamine include hypersensitivity reactions (immune
responses) that can irregularly be severe, such as Stevens-Johnson syndrome and
toxic epidermal necrolysis (two forms of the same life-threatening disease that
causes rash, skin peeling and sores on the mucous membranes), erythema
multiforme (a skin disorder with bulls-eye-shaped lesions), anaphylaxis (a
severe allergic reaction that may include difficulty breathing and shock) and
hyperphenylalaninemia (elevated concentration of the amino acid phenylalanine
in the blood), particularly when pyrimethamine is administered at the same time
as a sulfonamide.
“Pyrimethamine should not be used in patients with known
hypersensitivity to pyrimethamine or with documented megaloblastic anemia
because of folate (a naturally-occurring B vitamin) deficiency. Women who takes
pyrimethamine should not become pregnant. Patients should keep pyrimethamine
out of the reach of children.”
A small “starting” dose for toxoplasmosis is recommended in patients with
convulsive disorders in order to avoid the potential nervous system toxicity of
pyrimethamine. Pyrimethamine should be used with caution in patients with
impaired renal (kidney) or hepatic (liver) function or in patients with
possible folate deficiency, such as individuals with malabsorption syndrome,
alcoholism or pregnancy, and those receiving therapy, such as phenytoin (an
anti-epileptic drug), affecting folate levels.
The sponsor of the approved
generic version of the Daraprim Tablets is Cerovene Inc.
The FDA, an agency within the U.S. Department of Health and Human Services, protects the public health by assuring the safety, efficiency, and security of human and veterinary drugs, vaccines and other biological products for the human use, and medical devices. In addition, agency is responsible for the safety and security of our nation’s food supply, cosmetics, dietary supplements, products that give off electronic radiation, and for regulating tobacco products.
https://www.fda.gov/news-events/press-announcements/fda-approves-first-generic-daraprim