On 31-Mar-2020, FDA announced that ” As part of the Trump Administration’s all-hands-on-deck approach across public, academic and private sectors to combat the COVID-19 pandemic, the U.S. Food and Drug Administration stood up a new program to expedite the development of potentially safe and effective life-saving treatments.
The program, known as the Coronavirus Treatment Acceleration Program (CTAP), is using every tool at the agency’s disposal to bring new therapies to sick patients as quickly as possible, while at the same time supporting research to further evaluate whether these medical countermeasures are safe and effective for treating patients infected with this novel virus.
The FDA is announcing a new, comprehensive public-private approach to bring coronavirus treatments to market as fast as possible,” said HHS Secretary Alex Azar.
“As part of this new program, the FDA is cutting red tape, redeploying staff and working day and night to review requests from companies, scientists and doctors who are working toward therapies.
We are grateful to the men and women of the FDA who have been working in concert with industry and other parts of HHS to support potential coronavirus treatments for weeks now. Each day, President Trump’s all-of-America approach is making progress and providing new hope in our fight against the coronavirus
There are a large number of companies and researchers developing and evaluating COVID-19 related therapies. Given the urgent nature of the pandemic, under the FDA’s accelerator program, staff from the Center for Drug Evaluation and Research and the Center for Biologics Evaluation and Research are providing regulatory advice, guidance and technical assistance as quickly as possible. As part of this work, the FDA is triaging requests from developers and scientists seeking to develop new drug and biologic therapies, getting the relevant FDA staff in touch with them and providing rapid, interactive input to get studies underway quickly. For example, the FDA has reviewed study protocols within 24 hours in many cases and has reviewed single-patient expanded access requests generally within three hours. The FDA is also collaborating with federal partners, developers and researchers to create protocols that can be used across institutions and programs to streamline efforts.
Quickly after the emergence of this virus, we began working directly with federal health partners, academia and industry to advance medical countermeasures against COVID-19. Our staff continues to work across all sectors to expedite the development of numerous, innovative potential prevention and treatment approaches. We are also looking at pragmatic and expedited ways to make these products available to patients, while still ensuring the FDA’s standards are met,” said FDA Commissioner Stephen M. Hahn. “Accelerating the investigation of products that could potentially benefit people affected by the COVID-19 pandemic is one of the FDA’s highest priorities. We want to help patients by expediting promising treatments and are committed to maximizing our regulatory flexibility and proactively bringing the best innovators together to ensure we are getting the right treatments to the right patients at the right time.
To support these goals, the FDA has, among other things, redeployed medical and regulatory staff to serve on review teams dedicated to COVID-19 therapies, streamlined processes and operations for developers and scientists to send inquiries and requests and provided resources to health care providers and researchers to help them submit emergency requests to use investigational products.
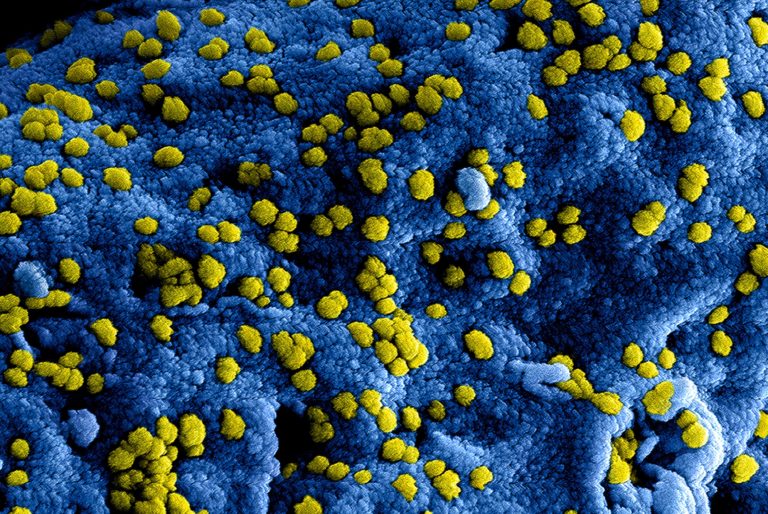
There are a variety of therapeutic areas being evaluated, including antiviral drugs like remdesivir that might treat the specific virus, as well as host targets, such as interleukin-6 (IL-6) receptor inhibitors that may be helpful in reducing lung inflammation and improving lung function in COVID-19 patients. There’s also interest in examining whether therapies such as convalescent plasma and hyperimmune globulin, antibody-rich blood products that are taken from blood donated by people who have recovered from the virus, could shorten the length or lessen the severity of the illness. Work is also ongoing to evaluate whether existing therapies such as chloroquine and hydroxychloroquine (with or without other medications) help treat patients with COVID-19.
The FDA also recognizes the potential for many different real-world data sources to complement traditional clinical studies and speed the process of evaluating the impact of potential COVID-19 therapies. To that end, the agency is advancing relationships with partners in the public and private sectors to rapidly collect and analyze information in areas such as illness patterns and treatment outcomes.
The FDA’s efforts to facilitate the development of COVID-19 therapies are focused on expediting the development of data on these medical countermeasures that can meet the agency’s world-respected gold standard for full FDA approval, which relies on data from adequate and well-controlled trials to most efficiently determine if an experimental treatment can safely and effectively benefit patients.
The FDA will continue to enhance and expand its work across the federal government and innovators in academia and industry to accelerate COVID-19 treatments and other medical countermeasures. The agency will outline additional information in the near future to provide a greater understanding of the full breadth of work in this area, to the extent permitted by confidentiality laws.
The FDA, an agency within the U.S. Department of Health and Human Services, protects the public health by assuring the safety, effectiveness, and security of human and veterinary drugs, vaccines and other biological products for human use, and medical devices. The agency also is responsible for the safety and security of our nation’s food supply, cosmetics, dietary supplements, products that give off electronic radiation, and for regulating tobacco products.
https://www.fda.gov/news-events/press-announcements/coronavirus-covid-19-update-fda-continues-accelerate-development-novel-therapies-covid-19