April 16, 2020: Alphamab Oncology announced that Jiangsu Alphamab Biopharmaceuticals Co., Ltd. (“Jiangsu Alphamab”), a wholly-owned subsidiary of the Company, received Safe to Proceed Letter from the US Food & Drug Administration (“FDA”) for its recombinant humanized PD-L1/CTLA-4 bispecific antibody KN046, to initiate Phase II clinical trial in anti-PD-(L)1 refractory or relapsed Non-Small-Cell Lung Cancer (“NSCLC”).
KN046’s Phase I clinical trials in Australia and China, along with multiple Phase II trials in China have shown a good safety profile and promising efficacy.
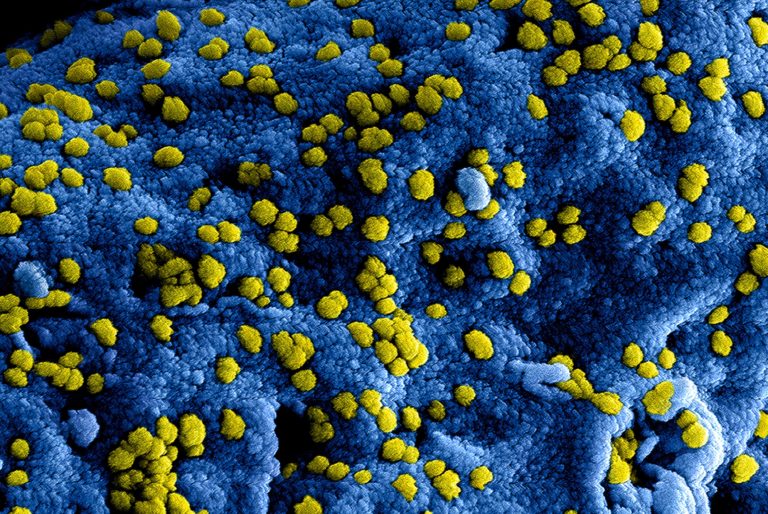
KN046 is a global first-in-class programmed death ligand 1 (“PD-L1”)/ cytotoxic T-lymphocyte-associated protein 4 (“CTLA-4”) bispecific antibody developed by the Jiangsu Alphamab. PD-(L)1 and CTLA-4 are the only two clinically validated immune checkpoints, and their combo therapy has been approved for the treatment of melanoma, colorectal cancer and kidney cancer, but application of the combo therapy has limited application due to its toxicity. Through innovative drug design, Jiangsu Alphamab has fused a novel CTLA-4 single-domain antibody with PD-L1 antibody to form KN046, a bispecific antibody with acceptable safety. KN046 has the capacity to block both PD-(L)1 and CTLA-4, effectively activate T-cells and strengthen anti-tumor immune activity.
KN046 is the only anti-PD-L1/CTLA-4 bispecific antibody drug in clinical development phase globally, and also Jiangsu Alphamab’s third drug candidates which have been approved to enter clinical trial in the United Sates. KN046 is currently undergoing multiple Phase II clinical trials for NSCLC, triple-negative breast cancer (“TNBC”), esophageal squamous cell carcinoma (“ESCC”) and pancreatic cancer. The result from these clinical trials is scheduled to be released in various occasions including international medical conferences. This Phase II clinical trial in the United States aims to evaluate the safety, tolerability and efficacy of KN046 monotherapy or in combination with chemotherapy in locally advanced unresectable or metastatic NSCLC.
Dr. Ting XU, Founder, Chairman and CEO of Alphamab Oncology commented, “We are unwaveringly committed to providing world class therapeutic biologics to global patients. Represented by KN046, our innovative bispecific antibodies pipeline has given us a head start to fulfill this mission. The IND approval from FDA is an important milestone for KN046’s the global development. We will accelerate clinical development on multiple oncology indications, and work hard towards an earlier market launch and provide cancer patients with a safe and more effective treatment option.”
KN046 is the world’s first recombinant humanized PD-L1/CTLA-4 bispecific antibody independently developed by Jiangsu Alphamab. Its innovative designs include: a proprietary CTLA-4 domain antibody with a significantly improved safety profile; a bispecific antibody fused with PD-L1 antibody; engineered to target the tumor microenvironment with high PD-L1 expression, and Treg clearing function. The preclinical and clinical study results of KN046 have shown promising efficacy and significantly reduced toxicity to human peripheral system, with the potential to become the backbone of next generation immuno-oncology therapy in the future.
Previously, KN046’s phase I clinical trials in Australia and China have shown a preliminary profile of good safety and promising efficacy, and several phase II clinical trials are ongoing in China for NSCLC, TNBC, ESCC and pancreatic cancer.
http://www.alphamabonc.com/en/html/news/2055.html