In module 1 i.e. induction of Medical Writing along with Types and Organisation name and What are skills required etc are covered. Have a look at the given link INTRODUCTION OF MEDICAL WRITING
Now, Let’s start with Module 2 i.e. Epidemiology and Evidence-Based Medicine
“Epidemiology is the analysis of the distribution and determinants in particular populations of health-related conditions or incidents, and the application of this study to the control of the health problems.
Epidemiology is the analysis (scientific, systematic , data-driven) of the distribution (frequency, pattern) and determinants (causes, risk factors) of health-related states and events (not just disease) in different populations (patient is group, individuals collectively viewed) and the application of this study (since epidemiology is a public health discipline) to the management of health problems.
Study
At its foundation, epidemiology is a medical discipline with strong scientific investigation methods.
Epidemiology is data-driven and is based on a clear and objective approach to data collection , analysis and interpretation.
Specific epidemiological methods continue to focus on careful observation and use of relevant reference groups to assess if what has been observed differs from what should be expected, such as the number of cases of disease in a specific area over a given period of time or the degree of exposure among people with the disease.
However, epidemiology also draws on approaches of biological , cultural, social , and behavioral sciences from other scientific fields, including biostatistics and informatics.
Even so, epidemiology is also defined as, and with good reason, the basic physics of public health.
- Epidemiology is a quantitative discipline focused on a working knowledge of the opportunities, statistics and sound methods of study.
- Epidemiology is a fundamental reasoning method focused on the creation and testing of theories based on scientific fields such as genetics, behavioral sciences, physics and ergonomics with a view to understanding health-related behaviors, states and events.
However, epidemiology is not just a research activity but an essential component of the public health, providing the foundation for directing practical and appropriate public health action based on this science and causal reasoning.
Distribution
Epidemiology is concerned with frequency and pattern of the health events in a population:
Frequency refers not only to the number of health incidents in the population, such as the number of cases of meningitis or diabetes, but also to the relation of this number to population size. The resulting rate allows for epidemiologists to assess the incidence of disease among various populations.
Pattern refers to health related incidents occurring by Time, location, person, etc. Timing trends can be annual, periodic, weekly, hourly, weekday versus weekend, or any other time breakdown that may influence the incidence of disease or injury.
Place patterns include geographic variation, differences between urban and rural, and places of work or school.
Personal characteristics include demographic factors that may be associated with disease risk, injury or disability such as age , sex , marital status, and socio-economic status, as well as behaviors and environmental exposure;
Characterizing health events by time , place and person are descriptive activities of epidemiology, discussed in more detail later in this lesson.
Determinants
Epidemiology is often used to search for the determinants, which are the causes and other factors that affect disease incidence and other events related to health.
Epidemiologists think illness isn’t. Occurrence randomly in a population, but occurs only when an person has the right accumulation of risk factors or determinants.
To search for these determinants, epidemiologists use analytic epidemiology or epidemiologic studies in order to provide the “Why” and “How” of such events.
They assess whether groups
with different rates of the disease differ in their demographic
characteristics, genetic or immunologic make-up, behaviors, environmental
exposures, or other so-called potential risk factors.
if possible, the findings provide sufficient evidence to direct prompt and efficient public health control and prevention measures.
Health-related
states or events
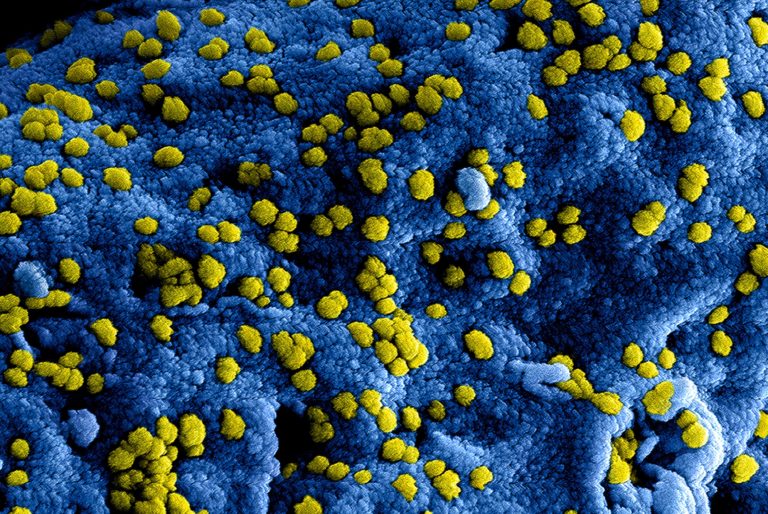
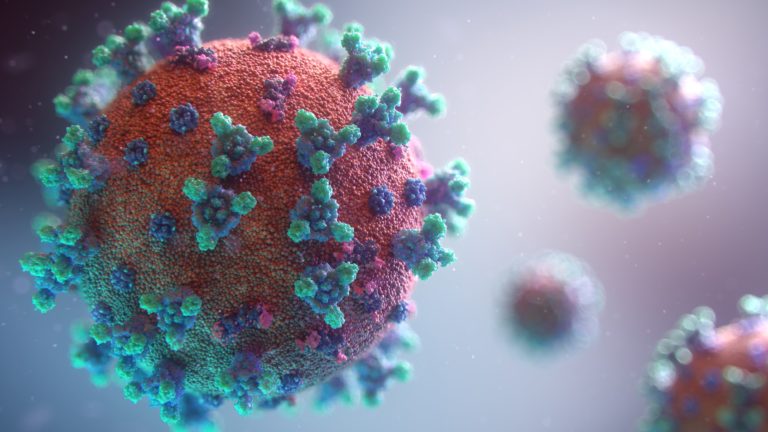
Epidemiology was originally focused exclusively on the epidemics of communicable diseases but was subsequently expanded to address endemic communicable diseases and non-communicable infectious diseases.
By the middle of the 20th century, infectious
illnesses, accidents, birth defects, maternal-child safety, occupational
health, and environmental health had been identified and applied to new
epidemiological approaches.
Then
epidemiologists started to look at health and wellness-related habits such as
the amount of exercise and the use of seat belt.
Nowadays, with the recent explosion in the molecular
methods, epidemiologists can make significant strides in examining genetic
markers of disease risk.
Certainly, the term health-related states or events may
be seen as anything that affects the well-being of a population.
nevertheless, many epidemiologists still use the term “disease” as shorthand for the wide range of the health-related states and events that are studied.
Specified
populations
Although epidemiologists and direct health-care
providers (clinicians) are both concerned with occurrence and control of
disease, they vary greatly in how they view “the patient.”
The clinician is anxious about the health of an
individual; the epidemiologist is anxious about the collective health of the
people in a community or population.
Or one can say, the clinician’s “patient” is the individual;
the epidemiologist’s “patient” is the community.
Therefore, the clinician and the epidemiologist have diverse
responsibilities when faced with a person with illness.
For example, when the patient with diarrheal disease presents, both are interested in establishing the correct diagnosis.
On the other hand, while the clinician usually focuses on treating and caring for the individual, the epidemiologist focuses on identifying the exposure or source that caused the illness; the number of other persons who may have been similarly exposed; the potential for the further spread in the community; and interventions to prevent additional cases or recurrences.
Application
Epidemiology is not just “the study of” health in the population;
it also involves applying the knowledge gained by the studies to the community-based
practice.
Like practice of medicine, the practice of epidemiology
is both a science and an art. To make the proper diagnosis and prescribe
appropriate treatment for the patient, the clinician combines medical
(scientific) knowledge with the experience, clinical judgment, and
understanding of the patient.
Likewise, the epidemiologist uses the scientific methods of the descriptive and analytic epidemiology as well as experience, epidemiologic judgment, and understanding of the local conditions in “diagnosing” the health of a community and proposing appropriate, practical, and acceptable public health interventions to manage and prevent disease in the community.
Evidence-Based Medicine
Evidence-based medicine (EBM) definition has generated considerable concern among health care professionals over the last decade.
According to definition Evidence-Based Medicine represents the integration of clinical expertise, patient’s values and best available evidence in the process of decision making related to patients health care.
Evidence-based medicine (EBM) is the deliberate, clear,
judicious, and fair use of new, best evidence in individual patient care
decision making.
EBM combines the best available scientific knowledge with
the clinical experience and patient beliefs. It is a trend aimed at increasing
the use of high-quality clinical research in making clinical decisions.
EBM needs the clinician’s new skills, including successful
literature-searching, and the application of structured standards of evidence
in clinical literature evaluation.
Evidence-based medicine practice is a lifelong,
self-directed, problem-based learning experience in which caring for one’s own
patients provides the need for clinically relevant knowledge about treatment,
prognosis, rehabilitation and other clinical and health-care concerns.
It’s not “cookbook” of recipes, but it offers
cost-effective and improved health care with its successful implementation. The
main distinction between evidence-based medicine and conventional medicine is
not that the evidence is taken into account by EBM when the latter does not.
Both takes into account evidence; however, EBM demands stronger evidence than
commonly used.
One of the greatest accomplishments in evidence-based
medicine has been the production in systematic reviews and meta-analyses,
methods by which researchers define several studies on a subject, isolate the
best ones and then critically examine them to summarize the best evidence
available.
Tomorrow’s EBM-oriented clinicians have three tasks: a) to
use summaries of evidence in clinical practice; b) to help establish and update
selected systematic reviews or evidence-based recommendations in their field of
expertise; and c) to enroll patients in the treatment, diagnosis, and prognosis
studies on which medical practice is based.
Medical awareness is growing every day, such that commonly
established theories easily become old and even an influx of scientific
evidence becomes difficult to pursue.
There are apparent challenges as physicians try to keep up with the latest developments reported in medical journals: for example, general practitioners can read 19 papers per day, and we know that many of them only have one hour a week for this.
Need for evidence-based approach in making decisions in the family medicine
The core of Family medicine in relation to doctor-patient.
One of the core aspects of this partnership is the decision-making process, which can differ from specific types of clinical decisions (e.g. the patient has a sore throat, larynx was red but without suppuration-why, it will prescribe antibiotics?) or (patient complained of frontal pain for two weeks, she was present when a patient walked-do you need to conduct CT of the head?), etc.
Difference between evidence- based medicine and evidence based health care
Having a distinction between these two words is worthwhile.
Evidence-based medicine is a physician’s systematic approach to decision taking
applicable to the actual patient.
Unlike this, Evidence-based health care is a much broader
term which requires advanced understanding of the beliefs, values and attitudes
of patients, families and physicians.
Evidence-based health care is also based on evidence, but primarily population-level data.
Gap between
research and practice
One of the primary reasons why there is a great interest in pursuing evidence-based medicine is the increasing number of cases where traditional medical practice can not keep up with the clinical evidence available.
For example , despite strong evidence during the seventies of the last century that treatment such as thrombolytic therapy and aspirin use was successful in treating acute myocardial infarction, it took nearly a decade for such therapies to become standard in clinical procedures for acute myocardial infarction patients.
Likewise, there are examples of complicated scientific research (evidences) being available everywhere, and its practical application. On the one hand, there is a lack of resolution that will synthesize the primary scientific researches and make systematic results.
On the other side, that indicates lack of ability of available evidences obtained in research which will gain relevant information which consumers of health services and medical professional needs to make decisions. In broader sense, that reflects lack of appropriate frames, systems and strategies which will more efficiently influence of professional conduct.
Complexity
of the primary health care (family medicine)
It is
understood that the patients come to the family doctor with poorly described
symptoms and wide clinical differences-the number of these patients in family
practice is definitely the largest.
They are so called symptoms of illness in the
“grey zone”, generally multiple complains of the patients on different organic
systems. Rarely that is a single problem.
The truth is
that it is only possible to solve a limited number of cases during the first
doctor-patient meeting. Family practitioner is also unable to plan patient
treatment because it is a case of complicated conditions and it is difficult to
schedule treatment.
For general
practice, the dynamic nature of research ensures that the patient needs
assistance in the dimension of the illness (feeling ill) for which there is no
clear proof of any intervention’s efficacy.
Gill and
colleagues’ study is based on a longitudinal review of series of doctor-patient
interactions, showing that high percentage (81 percent) of general practice
intervention can be backed by evidence from randomized controlled trials and
(or) compelling non-experimental evidence.
There is
also a need to explore how the dynamics of the doctor-patient relationship
within family medicine can be integrated.
One of EBM’s
key principles is the hierarchy of validating facts based on which judgment is
taken, meaning it is important to determine the importance of evidence before
making decisions.
According to that concept most important evidence, for example effectiveness of the single therapeutic mean, comes from the results of the multicenter, randomized, comparison, controlled clinical study.
Evidences of least value are based on the studies of the physiology functions and clinicians observations.
Classification
of evidence – information levels
Evidence-based
medicine categorizes different forms of scientific evidence and rates them out
of the numerous inequalities that bedeviled medical science according to the
extent of their liberation.
1.Evidences obtained by the meta-analysis of several randomized controlled research (RCR).
1b.Evidences
from only one RCR.
2a.Evidences
from well designed controlled research RCR.
2b.Evidences
from one quasi experimental research.
3.Evidences from the non experimental studies (comparative research, case study), according to some, for example Textbooks.
4.Evidences
from experts and clinical practice.
The principle of EBM emphasizes, that the foundation of any medical decisions regarding the optimal diagnostic or therapy procedure are scientific evidences from clinical research, and clinical experience and intuition are of great help, but not main basis in decision-making.
How to
start: 5 steps process for use of evidence oriented approach in family medicine
Where do family medicine doctors continue in their daily practice if they want to follow evidence-based approach? The McMaster University Community for Evidence-Based Medicine Resource defined the method that each individual physician will adopt in implementing this approach in 5 phases.
- Problem definition,
- Search for wanted sources of the information,
- Critical evaluation of information,
- Application of information of the patient,
- Efficacy evaluation of this application on a patient.
Step 1. Defining problem
Each doctor several times the day is in the position of making various medical decisions. Often in process of the medical decision-making occur questions such as: for and against the use of certain therapies, whether to use a diagnostic test or screening procedure, the risk or prognosis of the particular disease or cost-effectiveness of specific interventions.
It is clear that the already busy doctor, will not be able to answer in this way all the questions that come in practice and therefore must resort to the process of determining priorities, as well as refining issues that needs to be asked.
A
clinician starts his or her search for the best and newest data needed to solve
individual patient’s problem by formulating an answerable clinical question.
Good clinical question must be clear, directly focused on the problem, and
answerable by searching the medical literature.
PICO format
A
good clinical question should have four essential components structured in the
PICO format (Patient or problem, Intervention, Comparison, Outcome).
PICO
format:
- the patient or problem – who are the relevant patients, what kind of the problem we try to solve?
- the intervention – what is the management strategy, diagnostic test or exposure (drugs, diagnostic test, foods or surgical procedure)?
- comparison of interventions – what is the control or alternative management strategy, test or exposure that we will compare?
- the outcome – what are the patient-relevant consequences of the exposure in which we are interested?
Type of clinical question
The most common type of clinical question is about how to
treat a disease or condition. Such questions are questions about intervention.
Types of clinical questions:
- questions about intervention
- questions about etiology and risk factors
- questions about frequency and rate
- questions about diagnosis
- questions about prognosis and prediction
- question about cost-effectiveness
- question about phenomena
Step 2. Search for
wanted sources of information
After formulating the clinical question, which stems from a
concrete patient, the next step is to search for relevant evidence that will
provide the answer to the question.
This is not always easy, especially in the Family medicine, in which the problems caries the poorlydefined problems in the start.
Moreover, there are several sources of knowledge that may aid, including medical journals, coping with other family medicine concerns, looking for online records, and connecting with colleagues.
The ideal information source is valid (contains high quality
data), relevant (clinically applicable), comprehensive (has data on all
benefits and harms of all possible interventions), and is user-friendly (is
quick and easy to access and use).
Step 3. Critical
evaluation of the information
It is important to read it carefully when we decide which magazine to read, since not all of the published information is of equal quality and importance. Critical assessment of the papers is a process requiring thorough reading and review of the methods, contents and conclusions.
A key question that should be kept in mind is “Do I believe in the results enough that I’ll be ready to a similar approach, or in achievement of similar results with my patients?” Skills to obtain the ability of the critical evaluation should be learned and practiced as any other clinical skills.
Step 4. Application
of information of the patient
In practice, the fourth step in the process of using Evidence Based Medicine is the decision on how to apply the information acquired on the particular circumstances pertaining to each patient. This is possibly a critical, if not the most complicated, step in the process.
Now it is necessary to decide whether there is something in
relation to our patient because of which it would be necessary to discard the
acquired information.
The questions that we should ask before the decision to
apply the results of the study are:
Are the participants in the study similar enough to my
patient?
Is the treatment available and is the health care system prepared to fund it?
What alternatives are available?
Do the potential side effects of the drug or procedure
outweigh the benefits?
Are the outcomes appropriate to the patient? Does treatment conflict with the patient’s values and expectations?
When anything does not work, it is important to balance the potential harm from the gain and do all that in cooperation with the individual, where in practice our decision will be shared in the end.
Step 5. Efficacy
evaluation of EBM application on a patient
The final step is the evaluation of Evidence – based approach and efficiency of its application to a specific patient. When anything does not work, it is important to balance the potential harm from the gain and do all that in cooperation with the individual, where in practice our decision will be shared in the end.
If the data differ significantly, it would be necessary to investigate why some patients did not respond to the changes introduced in the expected way and what can be done to change it.
The EBM-oriented clinicians of the tomorrow have three tasks:
To use evidence summaries in the clinical practice;
To help develop and update selected systematic reviews or evidence-based guidelines in their area of the expertise; and
To enrol patients in studies of treatment, diagnosis and
prognosis on which medical practice is based.
Many epidemiological principles, methods and techniques are put into good use in EBM.
The EB “movement” is attractive in it’s use of clearly defined procedures, generalizing (not always explicitly) the application of good epidemiologic principles, methods, and techniques. Epidemiology now needs to help determine the use of an EB approach.”
https://www.cdc.gov/csels/dsepd/ss1978/lesson1/section1.html
https://en.wikipedia.org/wiki/Epidemiology
https://www.eupati.eu/pharmacoepidemiology/evidence-based-medicine/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3789163/
https://www.hopkinsmedicine.org/gim/research/method/ebm.html