December 07, 2022: “Updated results from the DESTINY-Breast03 Phase III trial showed that Enhertu (trastuzumab deruxtecan) demonstrated a statistically significant and clinically meaningful improvement in overall survival (OS) compared to trastuzumab emtansine (T-DM1) in patients with HER2-positive unresectable and/or metastatic breast cancer previously treated with trastuzumab and a taxane.
These results and primary results from the DESTINY-Breast02 Phase III trial will be presented today at the 2022 San Antonio Breast Cancer Symposium (SABCS), with the updated results from DESTINY-Breast03 simultaneously published in The Lancet.
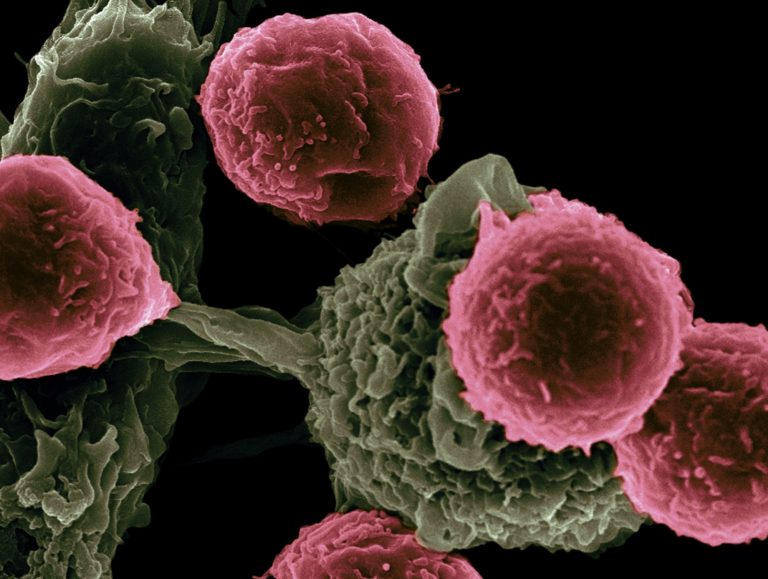
Enhertu is a specifically engineered HER2-directed antibody drug conjugate (ADC) being jointly developed and commercialised by AstraZeneca and Daiichi Sankyo.
In the key secondary endpoint analysis of OS for DESTINY-Breast03, Enhertu demonstrated a 36% reduction in risk of death versus T-DM1(based on a hazard ratio [HR] 0.64; 95% confidence interval [CI] 0.47-0.87; p=0.0037).
In both treatment arms, median OS was not yet reached (Enhertu [40.5-NE] versus T-DM1 [34.0-NE]) after a median duration of follow-up of 28.4 months for Enhertu and 26.5 months for T-DM1.
An estimated 77.4% of patients were alive in the Enhertu arm at two years compared to 69.9% of patients treated with T-DM1.
The observed survival benefit was consistent across all analysed subgroups, including patients with or without baseline brain metastases, with or without baseline visceral disease, those who were hormone receptor (HR)-positive or HR-negative, and regardless of prior pertuzumab or lines of systemic therapy.
Sara Hurvitz, MD, Medical Oncologist, Professor of Medicine, and Director of the Breast Cancer Clinical Trials Program in the Division of Hematology-Oncology at the David Geffen School of Medicine at UCLA, and Medical Director for the Clinical Research Unit at the UCLA Jonsson Comprehensive Cancer Center in Santa Monica, CA, said: “The main goals of therapy for advanced breast cancer are to control the disease and improve survival, and it is therefore critical to continue to improve upon existing treatment options, particularly in the metastatic setting.
For patients with HER2-positive breast cancer who experience disease progression following initial treatment in the metastatic setting, Enhertu has shown significant improvement in survival compared to T-DM1, further confirming this medicine as the new standard of care.”
Susan Galbraith, Executive Vice President, Oncology R&D, AstraZeneca, said: “The updated results for DESTINY-Breast03 showing that Enhertu extends patients’ lives and also delays progression by nearly two years reinforces our belief that this medicine has the potential to set a new standard of care for patients with HER2-positive metastatic breast cancer treated in the second-line setting.
Complemented by DESTINY-Breast02, we now have two Phase III trials in HER2-positive metastatic breast cancer showing patients in these trials have more disease-free time and live longer when they receive Enhertu versus the previous standard of care.”
Ken Takeshita, Global Head, R&D, Daiichi Sankyo, said: “The overall survival benefits shown in both the DESTINY-Breast03 and DESTINY-Breast02 trials further validate the role of Enhertu in potentially extending the lives of patients with previously treated HER2-positive breast cancer.
Additionally, median progression-free survival was four times longer with one in five patients showing no detectable signs of disease when treated with Enhertu compared to T-DM1 in DESTINY-Breast03, which is particularly impressive in the metastatic setting of HER2-positive breast cancer.”
With the additional follow-up in DESTINY-Breast03, Enhertu also continued to demonstrate a clinically meaningful improvement in progression-free survival (PFS) with a 22 month improvement in median PFS over T-DM1, reaffirming the statistically significant finding at the previous interim analysis.
The updated exploratory analysis was not tested for statistical significance and not powered to show differences between treatment arms.
In this exploratory post-hoc analysis, the median PFS for patients in the Enhertu arm was 28.8 months compared to 6.8 months for T-DM1, as assessed by blinded independent central review (BICR).
Confirmed objective response rate (ORR) was 78.5% in the Enhertu arm with 21.1% of patients demonstrating a complete response (CR) versus an ORR of 35.0% in the T-DM1 arm, where 9.5% of patients achieved a CR.
The median duration of response (DoR) was 36.6 months in the Enhertu arm and 23.8 months in the T-DM1 arm.
Summary of updated results: DESTINY-Breast03
| Efficacy Measure | Enhertu (5.4mg/kg)n=261 | T-DM1 (3.6mg/kg)n=263 |
|---|---|---|
| OS | ||
| Median OS (months) (95% CI) | Not reached (40.5-NE) | Not reached (34.0-NE) |
| Hazard ratio (95% CI) | 0.64 (0.47-0.87) | |
| p-value | p=0.0037i | |
| OS rate (%) (95% CI) | ||
| 12 months | 94.1 (90.4-96.4) | 86.0 (81.1-89.8) |
| 24 months | 77.4 (71.7-82.1) | 69.9 (63.7-75.2) |
| PFS by BICR | ||
| Median PFS (months) (95% CI) | 28.8 (22.4-37.9) | 6.8 (5.6-8.2) |
| Hazard ratio (95% CI) | 0.33 (0.26-0.43) | |
| p-value | p<0.000001i,ii | |
| Median PFS2 by investigatoriii | ||
| Median PFS2 (months) (95% CI) | 40.5 (40.5-NE) | 25.7 (18.5-34.0) |
| Hazard ratio (95% CI) | 0.47 (0.35-0.62) | |
| Confirmed ORR (%) (95% CI) | 78.5 (73.1-83.4) | 35.0 (29.2-41.1) |
| p-value | p<0.0001i,ii | |
| Complete Response (%) | 21.1% | 9.5% |
| Partial Response (%) | 57.5% | 25.5% |
| Stable Disease (%) | 18.0% | 41.8% |
| Progressive Disease (%) | 1.1% | 17.9% |
| Median DoR (months) (95% CI)iv | 36.6 (22.4-NE) | 23.8 (12.6-34.7) |
OS, overall survival; CI, confidence interval; PFS, progression-free survival; PFS2, second progression-free survival; BICR, blinded independent central review; ORR, objective response rate; DoR, duration of response
i Two-sided
ii Nominal p value. Updated exploratory analysis was not tested for statistical significance and not powered to show differences between treatment arms
iii From the time of randomisation to second progression
iv Based on BICR
The safety profile observed with Enhertu in DESTINY-Breast03 was consistent with previous clinical trials, with no new safety concerns identified.
The most common Grade 3 or higher treatment-related treatment-emergent adverse events (TEAEs) in the Enhertu arm were decreased neutrophil count (16.0%), anaemia (9.3%), decreased platelet count (7.8%) and nausea (7.0%).
There were 39 cases (15.2%) of treatment-related interstitial lung disease (ILD) or pneumonitis reported, as determined by an independent adjudication committee.
The majority (14.4%) were low grade (Grade 1 or Grade 2) with two Grade 3 (0.8%) events. No Grade 4 or Grade 5 ILD or pneumonitis events occurred.
DESTINY-Breast02 full results show significant improvements in PFS and OS versus chemotherapy in later-line HER2-positive metastatic breast cancer setting
In primary results from the DESTINY-Breast02 Phase III trial, Enhertu demonstrated a 64% reduction in the risk of disease progression or death in patients with HER2-positive unresectable and/or metastatic breast cancer previously treated with T-DM1 versus physician’s choice of treatment (trastuzumab plus capecitabine or lapatinib plus capecitabine) [HR=0.36; 95% CI 0.28-0.45; p<0.000001].
The median PFS for patients in the Enhertu arm was 17.8 months versus 6.9 months for those in the physician’s choice of treatment arm, as assessed by BICR.
Enhertu also showed a 34% reduction in the risk of death compared to physician’s choice of treatment (HR=0.66; 95% CI 0.50-0.86; p=0.0021) with a median OS of 39.2 months versus 26.5 months.
The data from DESTINY-Breast02 confirms the data seen in the DESTINY-Breast01 Phase II trial which supported the first approvals of Enhertu in patients with HER2-positive metastatic breast cancer who have received two or more prior anti-HER2-based regimens.
The safety profile of Enhertu in DESTINY-Breast02 was consistent with previous clinical trials with no new safety concerns identified.
The most common Grade 3 or higher treatment-related TEAEs in the Enhertu arm were decreased neutrophil count (10.6%), anaemia (7.9%), neutropenia (7.7%) and nausea (6.7%).
There were 42 cases (10.4%) of treatment-related ILD or pneumonitis reported, as determined by an independent adjudication committee.
The majority (9.1%) were low grade (Grade 1 or Grade 2) with three Grade 3 (0.7%) events, no Grade 4 events and two (0.5%) Grade 5 ILD or pneumonitis events occurring.”