“A protocol for clinical trials is a document outlining how a clinical trial should be performed, including the objective(s), design, methodology, statistical considerations and structure of the study to ensure participants’ health and the validity of the data collected.
What is Clinical Trial Protocol?
If you are involved in clinical investigation, you may need to contribute to the preparation of a clinical trial protocol.
A clinical trial protocol is a document explaining how to perform a clinical trial, including the purpose(s), design, methodology, statistical criteria, and structure of the trial to ensure the health of the patients and the validity of the data collected.
The protocol too provides the background and rationale for conducting the study and the research questions that it addresses, as well as considerations on the ethical issues.
According to the International Conference on Harmonization of Technical Criteria for the Approval of Pharmaceuticals for Human Use ( ICH), the structure and content of clinical trial protocols are standardized and meet the guidelines for good clinical practice (GCP) (first published in 1995, last revised in 2016)
Why is the clinical trial protocol needed?
The protocol is a key quality control tool for all aspects of a clinical trial, being necessary for several reasons:
- It ensures the health and safety of all study participants
- It provides a specific study plan
- It describes and manages the trial, and therefore it should be firmly followed by all the study investigators
- It guarantees the reliability of data, allowing the combination and comparison of the data across all investigators and/or study sites
- It notifies the study administrators, which frequently are a contract research organization (CRO)
- It is required to obtain ethical approval from the Research Ethics Committee or Institutional Review Board (IRB)
Related:
Content Guidelines and Templates
It is not uncommon to apply a protocol without critical details, or even whole sections; however, it should be avoided entirely. Create a list of what needs to be included in a clinical research protocol with reference to the relevant ICH guidelines (ICH E6 [R2]) and FDA guidelines.
Templates may also be accessible online (e.g., the joint NIH / FDA protocol template); however, to ensure compliance each template should be carefully checked against current regulatory requirements.
Sample Protocol Templates and Resources:
Protocol development assistance covering a wide-range of therapeutic areas is available. For cancer research protocol templates and additional guidance, please see Cancer Center Investigational Trials Resource Forms.
https://hub.ucsf.edu/protocol-development
Clinical trial Protocol Includes:
The ICH website lists the full list of the topics to be included in the protocol. Note that site specific information may be included in a separate agreement, and some of the information mentioned below may be included in other related protocol documents, such as a brochure for an investigator.
Depending on the anticipated study design, various specific guidelines were created, most of them providing a full list of items to be covered. You can access a standardized treatment template from the US National Cancer Institute’s Cancer Therapy Assessment System as an example here.
- Title page (general information)
Including protocol title; protocol identification number; date; potential amendments (more information about amendments in a following section); name and contact details of the sponsor, monitor, medical expert, investigator, and other institutions involved.
- Background information
Includes name and description of the investigational product(s); a summary of results from non-clinical and other clinical studies; known and possible risks and benefits; definition of route of administration and dosage; statement ensuring compliance with protocol, GCP and regulatory requirements; description of the population; references to relevant literature.
- Objectives/purpose
A detailed description of the objectives and the purpose of the trial.
- Study design
Including information about the primary and secondary endpoints, description of the nature of the experiment, description of bias minimization steps (including randomization and blinding), description of the medication and dosage schedule, estimated length of subject participation, description of discontinuation requirements, accountability procedures, etc. - Selection and exclusion of subjects
Explanation of inclusion, exclusion, and withdrawal criteria, as well as withdrawal procedures.
- Treatment of subjects
Information about treatment (product name, dose, dosing schedule, route, treatment period, follow-up), other permitted or not permitted medications/treatments, procedures for monitoring compliance.
- Assessment of efficacy
Specification of efficacy parameters, as well as methods and timing for their assessment, recording, and analysis.
- Assessment of safety
Specification of safety parameters; methods and timing for assessment, recording, and analysis of safety parameters; reporting and follow-up after adverse events.
- Statistics
Description of the statistical methods to be used; sample size; termination criteria; accounting procedures for incomplete, unused, and spurious data; reporting procedures for any deviations; selection of subjects to be included in the analyses.
- Direct access to source data/documents
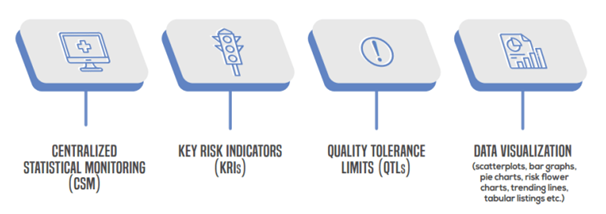
The sponsor will ensure that the protocol (or other written agreement) specifies that the investigator(s)/institution(s) must provide for trial-related monitoring, audits, IRB analysis and regulatory inspection(s), including direct access to the source data and records. - Quality control and assurance
Definition of the quality assurance and quality management processes implemented for ensuring data quality (including any training session, investigator supervision, instruction manuals, use of independent internal or external audit procedures, etc.). - Ethics
Definition of ethical issues relating to the court, describing the legal code enforcement. For example, you will clarify how you handle specific ethical issues appropriately and satisfy the appropriate regulatory criteria for the trial in an emergency situation (such as when the participant ‘s prior consent is not possible).You can read the EU document about ethical considerations for trials on medicinal products conducted with the paediatric population in this link.
- Data handling and record-keeping
This section ensures that the electronic data processing system(s) complies with the criteria for completeness, precision, reliability, and consistent intended performance defined by the sponsor. It should state that an independent data-monitoring committee has been set up to evaluate the trial ‘s progress.
- Financing and insurance
Details about the trial financing and the clinical trial participant’s insurance that is compulsory in many countries.
- Publication policy
Description of clinical data publishing policies ( e.g. papers, abstracts, posters, oral reports, and review articles published by peer-reviewed medical journals or delivered at scientific meetings and congresses), pledging adherence to GCP and related guidelines. (Note: topics 13-15 should be included in the protocol if not addressed in a separate agreement.)
- Project timetable/flowchart
Timeline description, including the planed start and end of the trial.
- References
- Supplements/appendices
Clinical trial Protocol: A team effort
- Protocols for clinical trials are not typically written by a single person. Instead, they are published by a multi-disciplinary team that also involves a medical expert, a statistician, a pharmacokinetics researcher, the supervisor of clinical testing, the project manager, and a scientific writer who incorporates all the contributions in a final article, among others.
The medical expert plays a leading role in research preparation, relating to sections such as study design, priorities and endpoints, selection criteria, and evaluation procedures. The medical professional also offers guidance on the use of parallel treatments or the guidelines for preventing dose escalation studies. The role of the medical expert is not normally outsourced.
The statistician conducts estimates for the sample size and research power (key to detect clinically relevant discrepancies between treatment groups) and contributes to the targets and endpoints being set. The statistician is responsible for carrying out all statistical procedures and ensuring the study’s possible variability is minimised. The role of the statistician can be outsourced to a temporary statistician or biostatistics consultant.
- The pharmacokinetic specialist assists in determining targets and endpoints, as well as in dosing protocols, defining the drug ‘s critical pharmacokinetic specifications.
This specialist also participates in the development of statistical methods for the assessment of pharmacokinetic data and in the determination of dosing frequencies from single to multiple ascending dose studies.
One can outsource the role of the pharmacokinetic expert.
- The Clinical Research coordinator contributes to clinical research management and logistics, including laboratory health and storage of samples.
In addition, the planner is also responsible for assessing the effectiveness of the various assessments, planning their timetable and definition. The position of coordinator of clinical research is not usually outsourced.
- Apart from managing data processing, the project manager is responsible for creating comprehensive timelines for the protocol and the research set-up specifications.
The project manager will also need to describe the requirements of the sponsor. The project manager job can be outsourced.
- Other people contributing to the clinical trial protocol include regulatory affairs specialists (that guarantee the adoption of all regulatory guidances, communicate with health authorities, and submit the Investigational Medicinal Product Dossier); laboratory staff (that handles samples and performs laboratory procedures); and the medical affairs/pharmacovigilance experts that manage the reporting of adverse events. Some of these roles can be outsourced.
The medical writer compiles the clinical trial protocol using feedback from the rest of the team, ensuring accuracy of the details in the entire text. They may outsource the role of the medical writer.
The SPIRIT Statement
In order to improve the content and quality of protocols, an international group of experts developed the Standard Protocol Items: Recommendations for Interventional Trials (SPIRIT) 2013 Statement.
The SPIRIT Statement provides guidance in the form of the checklist of recommended items to include in a clinical trial protocol and related documents.
The use of this guideline to write the study protocol optimizes the quality of the reporting and facilitates the peer review process. SPIRIT has created an electronic tool (SPIRIT Electronic Protocol Tool & Resource, SEPTRE) to help researchers to produce high-quality clinical trial protocols using SPIRIT guidance.”
Protocol deviations, violations and/or amendments
“Protocol deviations are characterized as unintended or unintentional changes to the protocol or non-compliance with the research protocol that do not increase the risk or decrease the benefit or have no significant impact on the rights, protection or welfare of the subject and/or the integrity of the data. Deviations in the protocol arise from the behavior of the subject or research staff.
Examples of the protocol deviations include a rescheduled study visit or failure to collect an ancillary self-report questionnaire. An example of protocol deviation is measuring vital signs prior to obtaining informed consent.
Protocol deviations should be distinguished from protocol violations involving unintended or unintentional protocol adjustments, or non-compliance with the protocol approved by the IRB, without prior sponsor and approval by the IRB. In general, violations increase the risk or decrease the benefit, affect the rights, health or welfare of the subject or the quality of the data.
Examples of protocol violations include the use of an insufficient informed consent, the enrollment of the subjects not meeting the inclusion and/or exclusion criteria, the use of forbidden medication, etc.
Protocol modifications that potentially impact the development of the study, the potential patient’s benefit, or may affect patient’s safety (including changes to the study objectives, study design, patient population, eligibility criteria, sample sizes, study procedures, or significant administrative aspects) require a formal amendment to the protocol.
Examples of the protocol changes that must be reported include any enhancement in drug dosage or duration of drug exposure, any important increase in the number of subjects to be enrolled, new test procedures, or the inclusion of a new investigator in multi-centric studies.
As an example, the Substantial Amendment Notification Form in the EU can be found here.
Alternatively minor corrections and/or clarifications that do not affect the way the study is conducted are considered administrative changes and should be documented in the memorandum.”
References:
https://hub.ucsf.edu/protocol-development
https://www.nuventra.com/resources/blog/best-practices-clinical-study-protocol-writing/