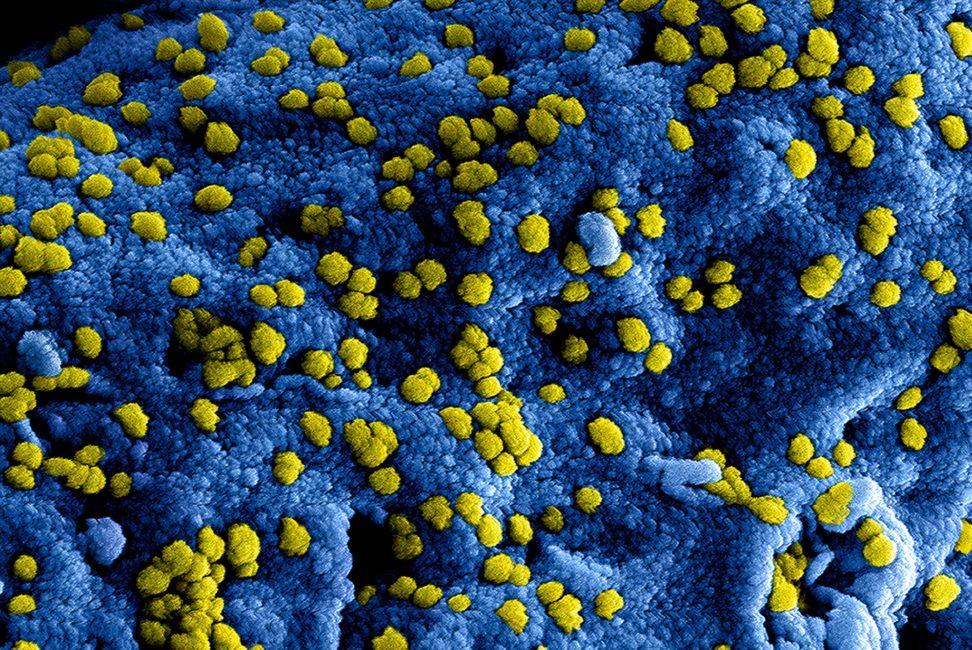
CAR-T cells are genetically engineered in order to express chimeric antigen receptors specially directed toward antigens on a patient’s tumour cells and then infused into the patient where they attack and kill the cancer cells.
Adoptive transfer of the T cells expressing CARs is a promising anti-cancer therapeutic because CAR-modified T cells can be engineered to target nearly any tumour-associated antigen.
GFRvIII is being targeted by the O’Rourke Laboratory in the treatment of glioblastoma. This approach has great potential in order to improve patient-specific cancer therapy in a profound way.
Early CAR-T cell research has focused on the blood cancer, first approved treatments use CARs that target the antigen CD19, present in B-cell-derived cancers such as acute lymphoblastic leukaemia (ALL) and diffuse large B-cell lymphoma (DLBCL).
Also, there are efforts in progress to engineer CARs targeting many other blood cancer antigens, including CD30 in refractory Hodgkin’s lymphoma; CD33, CD123, and FLT3 in acute myeloid leukaemia (AML); and BCMA in multiple myeloma. Solid tumours have been presented a more difficult target.
Identification of good antigens proved challenging: such antigens must be extremely expressed on the majority of cancer cells, but mostly absent on normal tissues. CAR-T cells are also not trafficked powerfully into the centre of solid tumour masses, and the hostile tumour microenvironment suppresses T cell activity.
Above diagram represents the process of chimeric antigen receptor T-cell therapy (CAR), this is a method of immunotherapy, which is a growing practice in the treatment of cancer.
The final product should be a production of equipped T-cells that can recognize and fight the infected cancer cells of the body.
1. T-cells (labelled as ’t’) are removed from the patient’s blood.
2. Then in a lab setting the gene that encodes for specific antigen receptors are incorporated into the T-cells.
3. Thus producing the CAR receptors (labelled as ‘c’) on the surface of cells.
4. The recently modified T-cells are then further harvested and grown in the lab.
5. After a certain time period, the engineered T-cells are then infused back into the patient.
Safety concerns: CAR-T cells are unquestionably a major breakthrough in the cancer treatment. However, there are serious side effects from CAR-T cells being introduced into the body, including cytokine release syndrome and neurological toxicity.
Because it is a comparatively new treatment, there is very little data about the long-term effects of CAR-T cell therapy. There are still concerns about long-term patient survival, as well as pregnancy complications in the female patients treated with CAR-T cells.
The most widespread issue behind treatment with CAR-T cells is cytokine release syndrome (CRS), a condition in which immune system is activated and releases an increased number of the inflammatory cytokines.
The clinical manifestation of this syndrome resembles sepsis with high fever, fatigue, myalgia, nausea, capillary leakages, tachycardia and other cardiac dysfunction, liver failure, and kidney impairment.
This syndrome occur in almost all patients treated with CAR-T cell therapy and in fact, the presence of CRS is a diagnostic marker that indicates the CAR-T cells are working as intended in order to kill the cancer cells.
Neurological toxicity is frequently associated with CAR-T cell treatment. Clinical manifestations include delirium, the one-sided loss of the ability to speak coherently while still having the ability to interpret language (expressive aphasia), lowered alertness (obtundation), and seizures.
During some clinical trials deaths caused by the neurotoxicity, the main cause of death from neurotoxicity is cerebral edema. Anaphylaxis is an expected side effect, as the CAR is made with the foreign monoclonal antibody and as a result, incites an immune response.
There is also the unlikely possibility that engineered CAR-T cells will themselves become transformed into cancerous cells during insertional mutagenesis, due to viral vector inserting the CAR gene into a tumour suppressor or oncogene in the host T cell’s genome.
Some retroviral (RV) vectors carry a lower risk than lentiviral (LV) vectors. However, both have the potential to be oncogenic.
https://www.cancer.gov/about-cancer/treatment/research/car-t-cells https://en.wikipedia.org/wiki/Chimeric_antigen_receptor_T_cell