Chimeric antigen receptor T cells (also known as CAR T cells) are T-cells that have been genetically engineered in order to produce an artificial T-cells receptor for use in immunotherapy.
Chimeric antigen receptors (CARs, also known as chimeric immunoreceptors, chimeric T cell receptors or artificial T cell receptors) are the receptor proteins that have been engineered to give T-cells the new capability to target a specific protein. The receptors are called chimeric because they combine both antigen-binding and T-cell activating functions into a single receptor.
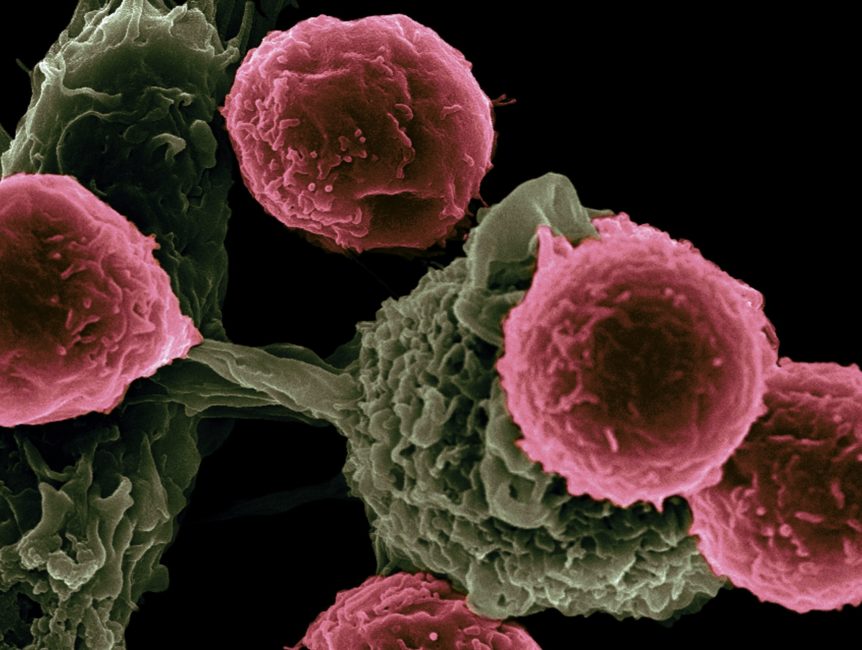
CAR-T cell therapy uses T cells engineered with CARs for the cancer therapy. The premise of CAR-T immunotherapy is to alter T cells to recognize cancer cells in order to more efficiently target and destroy them. Scientists harvest T cells from people, genetically modify them, then infuse the resulting CAR-T cells into patients to attack their tumors. CAR-T cells can be either derived from the T cells in a patient’s own blood (autologous) or derived from T cells of another healthy donor (allogenic). Once isolated from a person, these T cells are genetically engineered in order to express a specific CAR, which programs them to target an antigen that is present on the surface of tumors. For safety, CAR-T cells are engineered to be specific to an antigen expressed on a tumor that is not expressed on the healthy cells.
After the infusion of CAR-T cells into a patient, they act as a “living drug” against cancer cells. As they come in contact with their targeted antigen on a cell, CAR-T cells bind to it and become activated, then proceed to proliferate and becomec cytotoxic. CAR-T cells destroy cells through numerous mechanisms, including extensive stimulated cell proliferation, increasing the degree to which they are toxic to other living cells (cytotoxicity) and by causing the improved secretion of factors that can affect other cells such as cytokines, interleukins and growth factors.
Now Question is 1. How CAR-T cell produced? 2. How CAR-t cell treat Cancer? What are safety concerns? 3. What are Clinical studies and FDA approvals CAR-t cell therapy? 4. What is the structure of CAR Receptor? 5. How Evolution of CAR design takes place? So lets starts with the production of CAR-T cells
For the production of CAR-T cells the first step is the isolation of T cells from human blood. CAR-T cells may be manufactured either from the patient’s own blood (autologous treatment), or from the blood of a healthy donor(allogeneic treatment). The manufacturing process is the same in both cases; only the initial blood donor is different.
First, leukocytes are isolated using blood cell separator in a process known as leukocyte apheresis. Peripheral blood mononuclear cells (PBMC) are separated and then collected. The products of leukocyte apheresis are then transferred to the cell-processing center. In the cell processing center, specific T cells are stimulated so that they will aggressively proliferate and expand to large numbers. In order to driven their expansion, T cells are typically treated with the cytokine interleukin-2(IL-2) and anti- CD3 antibodies.
The expanded T cells are then purified and transduced with a gene encoding the engineered CAR via a retroviral vector, typically either an integrating gammaretrovirus (RV) or a lentiviral (LV) vector. These vectors are very safe in present times due to a partial deletion of the U3 region. The new gene editing tool CRISPR/Cas9 has recently been used as an alternative of retroviral vectors to integrate the CAR gene into specific sites in the genome.
The patient undergoes lymphodepletion chemotherapy earlier to the introduction of the engineered CAR-T cells. The depletion of number of circulating leukocytes in the patient upregulates the number of cytokines that are produced and reduces the competition for resources, which helps to promote the extension of the engineered CAR-T cells.